Compassion beyond the screen: Dr. Laura Desveaux’s research shows how compassionate health care can thrive in virtual care
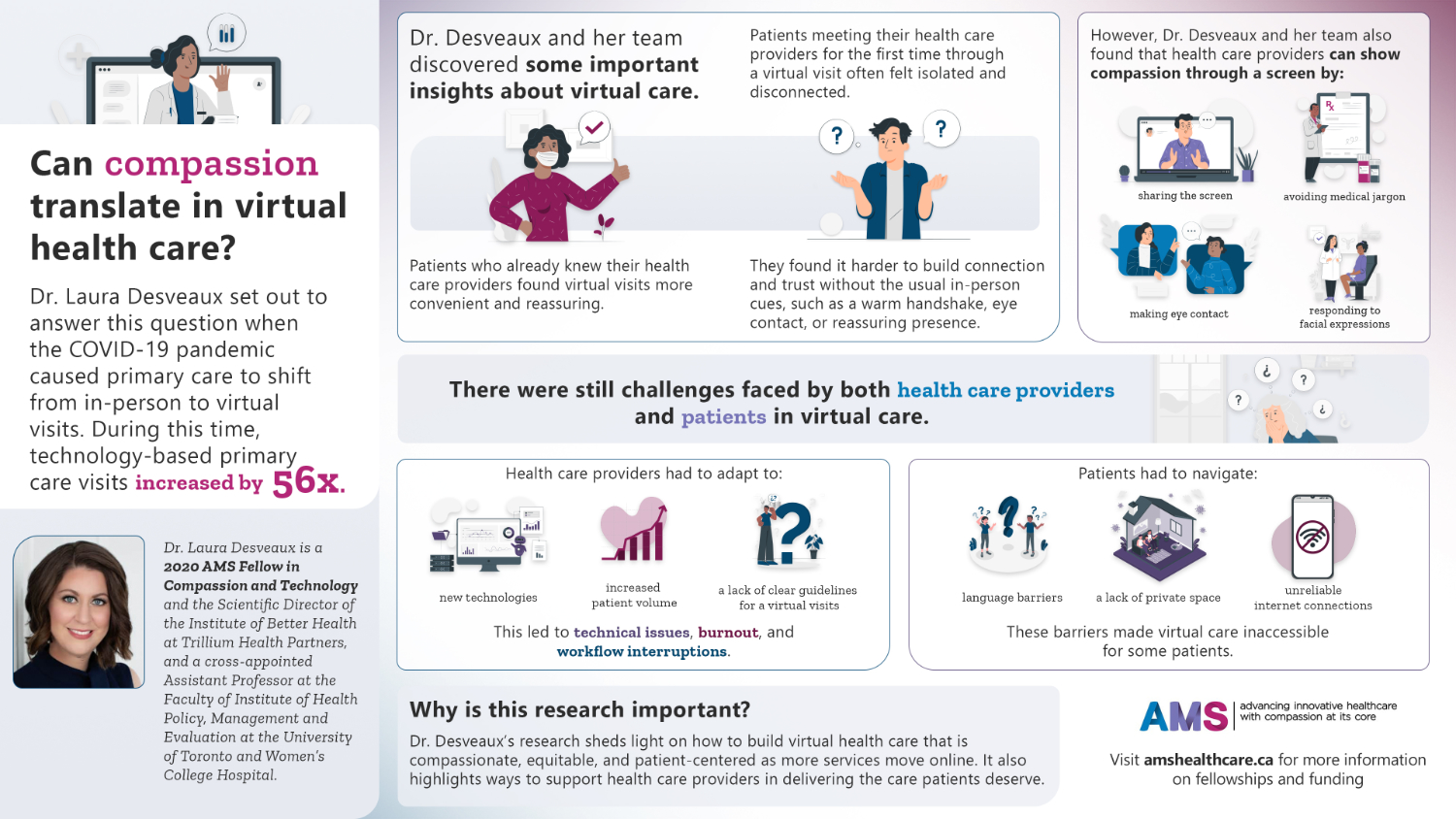
Ontario’s health care system experienced a seismic shift in the wake of the COVID-19 pandemic. Technology-based primary care visits soared 56-fold while in-person visits dropped by nearly 80%. Amid the rapid pivot to virtual care and the near immediate decline in social connectivity, a pressing question emerged: can compassionate care translate through a screen? After all, compassion is the foundation of trust, patient satisfaction, and quality care.,
For Dr. Laura Desveaux, the urgency of this question sparked a mission that sat at the intersection of her interests in implementation science and health innovation. She recognized that Canadians needed the shift to virtual care to be more than just functional—it had to feel human. As health care continues to evolve and make strides in integrating technology, the stakes are high. Patients deserve personalized, compassionate interactions and many felt the loss of human proximity and touch acutely during virtual appointments, while clinicians faced new challenges in reimagining how they work to deliver empathetic care over a screen.
“Healthcare is the business of human behavior. It’s humans connecting with humans, and everyone at the table makes decisions,” she explains, highlighting the delicate interplay between clinical skill, contextual cues, and emotional intelligence—and how they come together to create genuine human connection.
Supported by AMS Healthcare as a 2020 AMS Fellow in Compassion and Technology, Dr. Desveaux set out to understand the impact of virtual care on patient-provider relationships and the actions clinicians can take to translate the empathy and connection at the heart of compassionate health care into a virtual encounter.
Promises, pitfalls, and pivots to realize compassion in virtual care
As her research progressed, Dr. Desveaux’s team identified strengths and limitations in the new virtually mediated world of health care. Patients who already had an established relationship with their clinician were more likely to find virtual visits convenient and reassuring because they were built on a pre-existing connection. But for those meeting a provider for the first time, the experience left them feeling isolated or disconnected. These patients struggled to build connection and a foundation for trust without the usual cues of in-person visits such as a warm handshake, eye contact, or a reassuring physical presence.
Yet, in the midst of these challenges, Dr. Desveaux’s team heard from patients to identify the path forward. They defined the specific behaviors that clinicians can do in a virtual visit to convey empathy, even through a screen. Small, intentional actions like sharing the screen, avoiding medical jargon, making eye contact, and responding to facial expressions created a compassionate patient experience. These simple gestures showed that, when used thoughtfully, technology could augment compassionate care rather than making it obsolete.
Challenges in virtual care still remain for both clinicians and patients
The unforeseen shift to virtual care left many clinicians grappling with new technologies, larger patient volumes, and a lack of established guidelines for virtual interactions. This abrupt transition increased the risk of burnout, with providers facing technical disruptions, workflow interruptions, and the emotional strain of connecting through what was initially perceived as an impersonal medium.
Patients faced language barriers, a lack of private space, and unreliable internet connections that meant virtual care was an inaccessible option for many. Alongside numerous other studies, Dr. Desveaux’s research underscores the importance of an equity-centered approach to virtual care to ensure that it enhances the healthcare system’s overarching goal of providing compassionate and accessible care for all. As digital health technologies and AI continue to advance, Dr. Desveaux advocates for a thoughtful, intentional approach to integration.
“If we ask ‘what’ first, I think we’re constraining ourselves,” she says. “Why does something need to be different, and why are we integrating technology and AI in health care? You can’t operationalize the ‘how’ if you aren’t clear on the problem you’re solving for.”
Championing compassionate leadership in health care’s digital future
For her, the true power of technology lies in its potential to meaningfully support patients and clinicians, making health care more effective without losing its human touch.
Currently, Dr. Desveaux is taking a system perspective and seeking to understand how healthcare leaders can integrate compassion into technology implementation within their organizations. Since her AMS Fellowship, Laura has become the first North American member of the Coalition for Compassion in Healthcare.
Thanks to the support of the AMS Fellowship, Dr. Desveaux has cultivated a passion for identifying how leaders can create compassionate organizations and lead large-scale implementations that are rooted in compassion. The findings from her Fellowship project and the connections she has built within the AMS community have enabled her to pursue these deeper questions, exploring compassionate care in new and unexpected ways. AMS Healthcare’s commitment to curiosity and compassion has empowered her and other health leaders to shape the future of health care, keeping patient well-being and empathy at the forefront.
Dr. Laura Desveaux is the Scientific Director of the Institute of Better Health at Trillium Health Partners and a cross-appointed Assistant Professor at the Faculty of Institute of Health Policy, Management and Evaluation at the University of Toronto and Women’s College Hospital.
_______________
1 Glazier, R. H., Green, M. E., Wu, F. C., Frymire, E., Kopp, A., & Kiran, T. (2021). Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. Canadian Medical Association Journal, 193(6), E200–E210. https://doi.org/10.1503/cmaj.202303
2 Dewar, B., & Nolan, M. (2013). Caring about caring: Developing a model to implement compassionate relationship-centred care in an older people care setting. International Journal of Nursing Studies, 50(9), 1247–1258. https://doi.org/10.1016/j.ijnurstu.2013.01.008
3 Tehranineshat, B., Rakhshan, M., Torabizadeh, C., & Fararouei, M. (2019). Compassionate care in healthcare systems: A systematic review. Journal of the National Medical Association, 111(5), 546–554. https://doi.org/10.1016/j.jnma.2019.04.002
_______________
Read Dr. Laura Desveaux’s Fellowship Publications:
Rouleau G, Wu K, Parry M, Richard L, Desveaux L. Providing compassionate care in a virtual context: Qualitative exploration of Canadian primary care nurses’ experiences. Digit Health. 2024 Jan 9;10:20552076231224072. doi: 10.1177/20552076231224072.
Desveaux L, Wu K, Rouleau G, Srinivasan D, Azavedo R, Dang Nguyen M, Martin D, Steele Gray C. Building Compassionate Experience Through Compassionate Action: Qualitative Behavioral Analysis. JMIR Form Res. 2023 May 31;7:e43981. doi: 10.2196/43981.
Wu K, Dang Nguyen M, Rouleau G, Azavedo R, Srinivasan D, Desveaux L. Understanding how virtual care has shifted primary care interactions and patient experience: A qualitative analysis. J Telemed Telecare. 2023 Apr 18:1357633X231167905. doi: 10.1177/1357633X231167905. Epub ahead of print.